The True Story of the Government Programs That Tried to Build an Atomic Heart
And the craziest part of the atomic artificial heart program wasn't the atomic part.

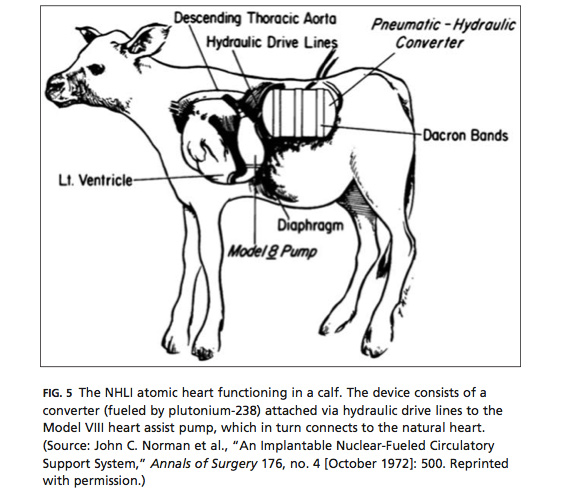
In 1967, the National Heart Institute and the Atomic Energy Agency began a ten-year effort to develop an artificial heart powered by plutonium-238. The atomic hearts would have pumped human blood with the energy provided by the radioactive decay of that isotope. The effort failed thanks to technical challenges, intra-governmental infighting, and the souring of the public mood about both medical devices and atomic energy, but it remains a fascinating episode at the confluence of two grand American dreams.
This is the story told by Shelley McKellar, who teaches the history of medicine at at the University of Western Ontario in the most recent issue of the quarterly journal Technology and Culture.
The Federally funded programs continued for a decade, sometimes at cross-purposes, and they foreshadowed the rhetoric that came to surround later attempts at creating other types of artificial hearts in the 1980s. There are lessons to be learned, McKellar implies, about how people receive a particular technology changes along with the social and regulatory environment. Ideas that make sense one decade can seem totally ridiculous ten years later.
But, you might be asking yourself, "What in the hell was anyone even thinking trying to stick a radioisotope generator into a human being's chest cavity?"
Fair question.
If you take the goal for an artificial heart to be the true replacement of the human heart in perpetuity, then power becomes a primary concern, trumping all other engineering constraints. When contractors like Westinghouse Electric and McDonnell-Douglas offered bids for the government work, they made sure to note the atomic solution as the only possibility.
"Each proposal declared the radioisotope-powered engine as the only possible energy solution for a completely implantable device." McKellar explained. "The ideal implantable device meant no external lines or connections from the patient to outside power sources and a ten-year reliability span. By comparison, conventional batteries required recharging multiple times each day from an external source and would need to be explanted from patients every two years."
And, if you're a promoter of the value of radioisotopes in all things, then you might go looking for places where power is a primary concern. As one William Mott, who became the project coordinator the Atomic Energy Commission's atomic heart program put it, "We were always on the alert for new problems to match with our solutions."Looking back, it's fascinating how confident the scientists of the time were that the engineering challenges of embedding a radioactivity-powered device into a body could be overcome. The NHI and AEC battled over the proper way of conducting the research: the NHI created a non-atomic intermediary device that they implanted into animals, while the AEC promoted an all-at-once design strategy. But both agencies saw the problems as fundamentally soluble.
With the benefit of 50 years of hindsight, we know that, so far at least, there is no "ideal implantable device." Total artificial hearts (as distinguished from heart assist devices) are, at best, a stopgap measure. They're used to as a last-ditch bridge measure while patients await transplants of other human hearts. We've learned a lot of other things about cardiology in the last 50 years, but one thing remains: nothing we can make comes close to working as well as your heart except another human heart.
That is to say: The craziest part of the atomic artificial heart program wasn't the atomic part.